Abstract:
This paper summarizes the clinical outcomes and biomechanical impacts of a prospective study on the Icarus Ascender brace in alpine skiers with patellofemoral osteoarthritis (PFOA), conducted by the Steadman Philippon Research Institute (SPRI) in Vail, CO. Participants wore the brace while skiing, reporting significant improvements in pain and muscle activation patterns. VAS pain scores decreased by an average of 44%, with 90% of participants experiencing pain reduction. EMG data revealed reduced quadriceps activation, suggesting that the brace effectively unloads the patellofemoral joint. These findings show promising results for the clinical efficacy of the Ascender in managing patellofemoral pain in skiing.

Introduction:
Knee osteoarthritis (OA) is a prevalent and debilitating condition, affecting over 14 million adults in the United States.1,2 Patellofemoral OA (PFOA) is by far the most prevalent, accounting for a majority of symptomatic OA cases. Epidemiological studies indicate that over 50% of symptomatic OA cases involve the PF compartment.3 Studies on OA further corroborate this, where 94% of knee pain patients with radiographic OA involved the patellofemoral compartment. Less than 6% of cases had isolated tibiofemoral compartment OA.4
PFOA treatment options remain limited, especially for patients not suited for surgical interventions. The utility of bracing in improving PFOA symptoms has been insufficiently explored—this study investigates the impact of a novel patellofemoral unloader brace on symptom alleviation and EMG-based muscle activation in skiers with PFOA.
Skiing and snowboarding place significant demands on the patellofemoral joint and the entire extensor mechanism, including the quadriceps and co-contracting muscles. Various common motions during skiing and snowboarding subject the patellofemoral joint to intense stress, such as when a skier jumps, lands, or aggressively turns. These motions are associated with impulse forces and rapid decelerations that generate high levels of pressure within the joint.5 This pressure is amplified by the extensor mechanism, where the quadriceps play a crucial role in absorbing and distributing these forces.6
Methods:
This prospective study enrolled 10 skiers with documented PFOA and anterior knee pain. All participants underwent biomechanical testing on a ski slope at Copper Mountain Resort, Colorado.
Skiers were fitted with an Ascender knee brace by Icarus Medical, and a Noraxon Ultium EMG system consisting of 3 electromyography (EMG) sensors to measure muscle activation and 3 inertial measurement units (IMU) capable of measuring joint kinematics and flexion angles. PRO (patient-reported outcomes) pain scores were evaluated after completion of each testing session under two brace conditions:
- 0 lbs unloading force (quadriceps unloading mechanism disengaged).
- 25 lbs unloading force (estimated, quadriceps unloading mechanism engaged).
Differences in knee kinematics, muscle activation, and PRO pain scores will be compared between groups.
Results:
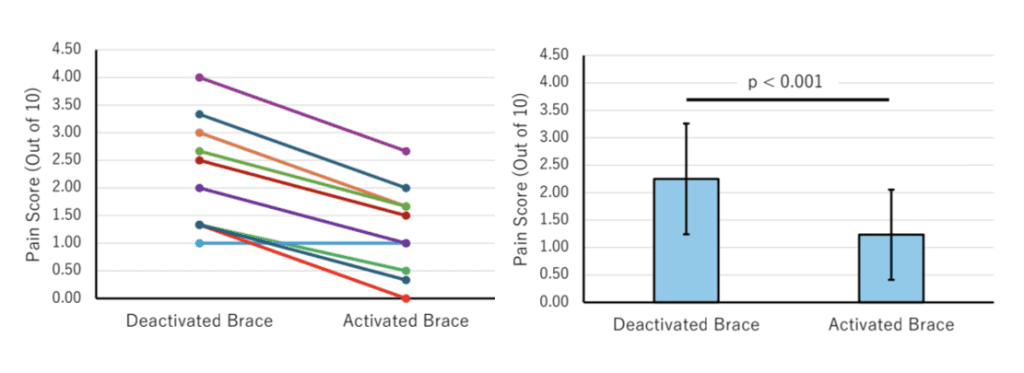
Pain Scores
90% of participants reported decreased pain with the unloading mechanism engaged, with an average 44% reduction in pain on the VAS pain scale from 2.25 to 1.25 (p < 0.001).
EMG Data
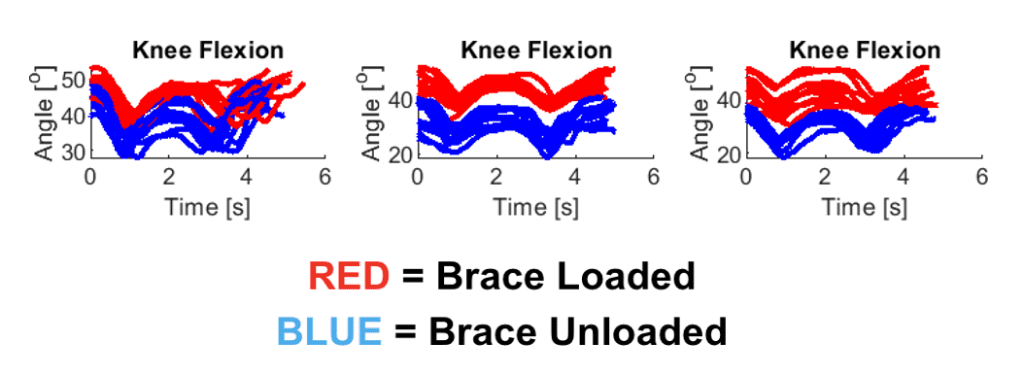
EMG data was collected on the 10 skiers in this study and analysis is underway, and will be reported in 2025. In a separate pilot study, SPRI collected EMG data in 2022 from a single skier that revealed decreased activity in the vastus medialis, vastus lateralis, and rectus femoris with the brace tensioned/loaded, as indicated by the EMG activity data in red in Figure 3. A decrease in extensor muscle activation is indicative of reduced patellofemoral joint stress.6
Increased Knee Flexion Angle
This skier a achieved significantly greater knee flexion angles while wearing the tensioned Ascender in 3 trials—an indicator of improved knee function and mobility.
Discussion:
The results indicate that skiers with PFOA can benefit both symptomatically and functionally from a patellofemoral unloader. The 44% improvement in VAS pain scores, increased knee flexion angles, and concurrent decrease in extensor mechanism activation are clinically significant results that highlight the viability of Ascender bracing as a successful, conservative treatment option for active patients.
The Ascender knee brace, by providing dynamic quadriceps unloading during knee flexion, addresses biomechanical challenges unique to the patellofemoral joint. The brace provides variable and dynamic extension assistance, reducing quadriceps activation and transferring load from the knee joint to the brace frame. This substantially reduces the pressure observed in the patellofemoral compartment (and medial and lateral tibiofemoral compartments). By mechanically reducing joint stress, the brace offers a targeted approach to managing pain and improving mobility. The stress in the patellofemoral joint is largely defined by the forces generated by the quadriceps muscles.6 This is supported by our understanding of the forces influencing the joint (see The Math Behind Patellofemoral Joint-Unloading).7 A reduction in the quadriceps’ EMG activity, which is representative of a reduction in its pulling force, is an indicator of reduced patellofemoral joint pressure. This reduced joint pressure is a game-changer for PFOA patients, and cannot be accomplished in the same way by traditional offloaders because they lack an extension-assisting force.
The study showed that the brace provided greater pain relief for individuals who had higher initial pain levels, suggesting that those with more severe symptoms may experience greater benefits. This is supported by other studies on the Ascender, such as the prospective study being conducted by Rush University Medical Center in Chicago, IL, where participants’ initial VAS pain scores were 4.04 (p<0.001) and improved by 59.2%, on average.
The increased knee flexion angle is a great standalone outcome of the study, suggesting that skiers with anterior knee pain experienced increased mobility while wearing the brace. However, it’s important to note that this occurred in conjunction with a reduction in EMG activity—suggesting that patellofemoral pressure decreased despite the notable increase in knee flexion. This is an impressive outcome considering the direct relationship between knee flexion, quadriceps contraction, and increased patellofemoral pressure.8,9 In summary, despite the increased knee flexion, quadriceps activation did not increase—suggesting that the Ascender can improve knee mobility while simultaneously reducing patellofemoral compartment pressure.
Conclusion:
The findings of this study underscore the potential of the Icarus Ascender knee brace as an effective, conservative intervention for individuals with PFOA, particularly those who engage in high-stress activities such as skiing. The brace’s capacity to reduce patellofemoral joint pain and stress, as evidenced by a 44% reduction in VAS pain scores and decreased quadriceps activation, supports its clinical efficacy. Additionally, the increased knee flexion angles observed in participants highlight its role in enhancing functional mobility without exacerbating joint stress. These outcomes suggest that the Ascender not only mitigates pain, but also improves biomechanical efficiency, providing a promising non-surgical treatment option for active individuals with symptomatic PFOA. Further research with larger sample sizes and diverse activity profiles is warranted to corroborate these findings and explore the brace’s broader applicability across different patient populations and activities.
Bibliography:
1. Deshpande, B. R. et al. Number of Persons With Symptomatic Knee Osteoarthritis in the US: Impact of Race and Ethnicity, Age, Sex, and Obesity. Arthritis Care Res. 68, 1743–1750 (2016).
2. Cross, M. et al. The global burden of hip and knee osteoarthritis: estimates from the global burden of disease 2010 study. Ann. Rheum. Dis. 73, 1323–1330 (2014).
3. Hart, H. F., Stefanik, J. J., Wyndow, N., Machotka, Z. & Crossley, K. M. The prevalence of radiographic and MRI-defined patellofemoral osteoarthritis and structural pathology: a systematic review and meta-analysis. Br. J. Sports Med. 51, 1195–1208 (2017).
4. Duncan, R. C., Hay, E. M., Saklatvala, J. & Croft, P. R. Prevalence of radiographic osteoarthritis–it all depends on your point of view. Rheumatol. Oxf. Engl. 45, 757–760 (2006).
5. Velasquez Hammerle, M. V., Roy, E. D., Gerber, A. R. & Tanaka, M. J. Patellofemoral disorders in winter sports. J. Cartil. Jt. Preserv. 3, 100140 (2023).
6. Besier, T. F., Gold, G. E., Beaupré, G. S. & Delp, S. L. A modeling framework to estimate patellofemoral joint cartilage stress in vivo. Med. Sci. Sports Exerc. 37, 1924–1930 (2005).
7. The Math Behind Patellofemoral Joint-Unloading: Force Vectors Explained -. Icarus Medical https://icarusmedical.com/technical-briefings/the-math-behind-patellofemoral-joint-unloading-force-vectors-explained/.
8. Loudon, J. K. BIOMECHANICS AND PATHOMECHANICS OF THE PATELLOFEMORAL JOINT. Int. J. Sports Phys. Ther. 11, 820–830 (2016).
9. Becker, R. & Awiszus, F. Physiological alterations of maximal voluntary quadriceps activation by changes of knee joint angle. Muscle Nerve 24, 667–672 (2001).
