Medicare has finalized an important update to the Knee Orthoses Local Coverage Determination that expands coverage for knee braces used to treat osteoarthritis of the knee.
Under the revised policy, objective joint instability is no longer required to prescribe a knee orthosis. This change addresses a long-standing limitation that previously restricted coverage to patients with documented instability, recent injury, or prior surgery.
Overall, the update more accurately reflects how knee osteoarthritis is treated in everyday clinical practice and acknowledges knee bracing as a conservative treatment option.
What Changed and Why It Matters
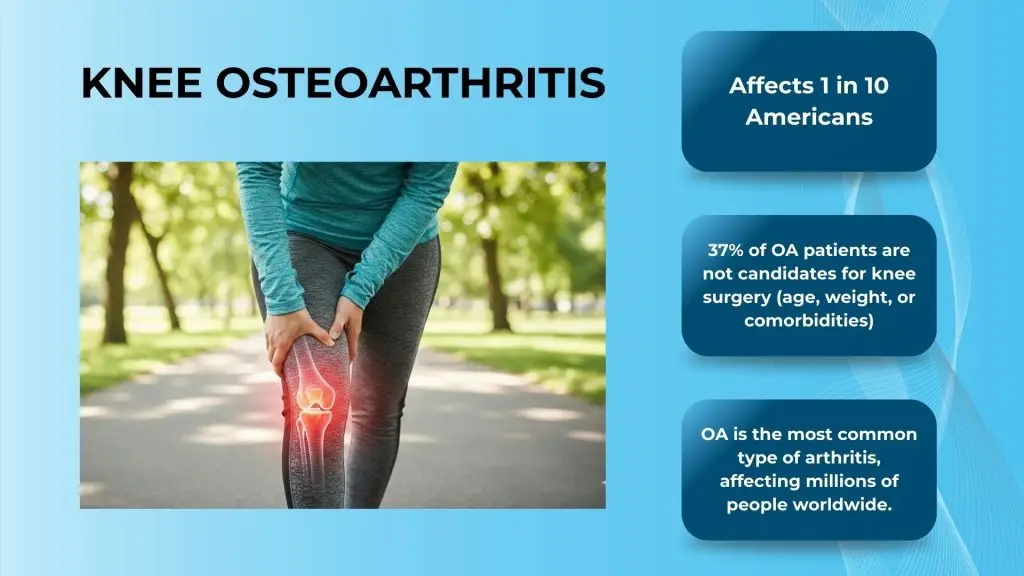
For years, many patients with medial or lateral compartment knee osteoarthritis were unable to receive Medicare coverage for unloader style knee braces, even when bracing was clinically appropriate and supported by evidence. This included patients whose symptoms were driven by pain and functional limitation rather than measurable joint laxity.
With the revised LCD, Medicare now allows coverage to be based on osteoarthritis related pain and functional impairment rather than instability alone. This expands access to non-surgical care and supports earlier intervention for a broader group of patients.
For clinicians, it also removes a common barrier when recommending knee bracing as part of an osteoarthritis treatment plan.
Who May Qualify Under the Revised Policy
- The patient is ambulatory and able to bear weight
- The patient experiences pain or functional limitation related to knee osteoarthritis
- The knee brace provides varus or valgus adjustment to address compartment loading
- The patient is willing to use the orthosis as part of their care plan
Objective joint instability is no longer required when these clinical criteria are satisfied.
What You Need to Know About Documentation
- Confirmation of the patient’s ambulatory status
- Description of pain, mobility limitations, or functional impact related to osteoarthritis
- Findings from a physical examination of the affected knee or knees
- Imaging that demonstrates arthritic changes consistent with medial or lateral tibiofemoral osteoarthritis
- Documentation that the patient understands and is willing to use the knee orthosis
Medicare has clarified that the patient’s willingness to use the brace may be documented by either the treating practitioner or the orthotist or prosthetist.
What This Means in Clinical Practice
- Experience activity-related knee pain
- Have difficulty with daily function or mobility
- Are seeking conservative, non-surgical treatment options
- May not yet be candidates for joint replacement
Knee orthoses with varus or valgus adjustment can help reduce load on the affected compartment, support functional movement, and improve comfort during daily activities.

When the Policy Takes Effect
The revised Knee Orthoses LCD applies to Medicare claims with a date of service on or after January 25, 2026. Until that date, the existing requirements remain in effect. Clinicians, orthotic providers, and billing teams may want to begin reviewing workflows and documentation practices now to ensure alignment once the policy takes effect.
If you would like to learn more here is the link to the LCD and pending Policy Article. questions related to patient eligibility, product selection, or the ordering process, the Icarus Medical team is available to help.





